Emily J. Carter¹*, Michael R. Thompson¹, Laura S. Martinez¹
¹ Department of Microbiology and Immunology, School of Medicine, University of Cambridge, Cambridge CB2 1TN, United Kingdom
* Correspondence: Emily J. Carter, Department of Microbiology and Immunology, School of Medicine, University of Cambridge, Cambridge CB2 1TN, United Kingdom.
Email: [email protected]
Abstract
The advent of antibiotics in the 20th century revolutionized modern medicine, rescuing millions of lives from previously fatal infections. However, over the decades, microbes have progressively evolved acquired antimicrobial resistance (AMR) as a result of sustained selective pressure brought about by the excessive and inappropriate application of these drugs. The spread and acquisition of AMR predominantly occur through human-to-human contact, both inside healthcare systems and in community settings. A broad range of interconnected determinants from clinical practices to agricultural use influence the emergence of resistant strains via diverse molecular resistance mechanisms. A particularly concerning driver has been the unregulated incorporation of antimicrobials in livestock feed, which accelerates resistance development. Today, antimicrobial-resistant pathogens have reached alarming global proportions, creating a silent pandemic that poses unprecedented risks to public health. Treatment options for infections caused by resistant organisms remain scarce, often leading to higher levels of morbidity, mortality, and significant healthcare expenditures. This crisis is further exacerbated by the stagnant pipeline of novel antimicrobials, which is unable to meet the escalating demand for effective therapies against multidrug-resistant pathogens. Urgent interventions must therefore prioritize robust surveillance systems, restriction of over-the-counter antibiotic sales, reduction of antimicrobial use in food production, equitable access to essential medicines, vaccines, diagnostics, and the enforcement of strong policy frameworks. Coordinated efforts across local, national, and international levels are indispensable. Without such measures, the post-antibiotic era—once regarded as a distant dystopia—may become an inevitable reality of the 21st century. This review underscores the mechanisms underpinning microbial resistance, the principal drivers of AMR, and the critical strategies required to mitigate its spread.
Keywords: antibiotics; antimicrobial resistance; resistance mechanisms; resistance drivers; strategies to combat AM
© The Author(s) 2025. Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third-party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc-nd/4.0/
INTRODUCTION
Antibiotics, often described as “magic bullets” against bacterial pathogens, are regarded as one of the most groundbreaking medical achievements of the 20th century. Their discovery and widespread application fundamentally reshaped therapeutic practices and continue to safeguard millions of people from life-threatening infections. Beyond clinical use, antibiotics have also been widely applied in agriculture, particularly in animal husbandry and food production, serving as preventive agents in numerous low- and middle-income countries for decades [1]. However, the extensive and frequently inappropriate utilization of these agents has fueled the emergence of antimicrobial resistance (AMR). This phenomenon occurs when microorganisms—including bacteria, viruses, fungi, and parasites—adapt to survive exposure to drugs specifically designed to eliminate them. Infections caused by resistant organisms are not only more difficult to manage, but they also heighten the risk of severe complications and mortality.
Antimicrobial agents comprise several categories—antibiotics, antifungals, antivirals, disinfectants, and preservatives—each of which either suppress microbial proliferation or eradicate pathogens. Among these, antibiotics remain the most extensively employed, particularly against bacterial infections, and their resistance is more frequently documented than for other antimicrobial classes. AMR represents a natural evolutionary adaptation in which organisms acquire genetic changes enabling survival under selective drug pressure. To withstand this pressure, bacteria develop multiple mechanisms to neutralize the effect of antibiotics, thereby rendering these agents ineffective [2]. In many developing countries, the widespread and uncontrolled use of antibiotics has provided bacteria ample opportunities to evolve resistance, culminating in substantial increases in disease burden, morbidity, and mortality [3–5]. The global escalation of resistant infections has reached a critical level in the 21st century, with AMR now described as a “silent pandemic” demanding urgent public health interventions [6].
Crucially, antibiotic resistance does not respect geographic or demographic boundaries—it can arise in any region and affect individuals of all ages. Presently, AMR poses one of the gravest challenges not only to human health but also to global food security [7]. Its emergence and dissemination are shaped by a complex web of interconnected factors spanning healthcare, agricultural practices, pharmaceutical waste, environmental contamination, trade, and economic dynamics, making AMR one of the most multifaceted threats to global health [8]. The accelerated worldwide spread of multidrug-resistant organisms—often referred to as “superbugs”—has further amplified concerns. The World Health Organization (WHO) now recognizes AMR as one of the three most critical global health risks. In fact, antimicrobial-resistant infections are already the third leading cause of mortality globally, following cardiovascular diseases [9]. A landmark study reported that in 2019 alone, 1.27 million deaths were directly attributed to AMR, while nearly 5 million deaths were associated with drug-resistant infections. Projections indicate this toll could rise to 10 million deaths annually by 2050, surpassing cancer as a leading cause of mortality [10]. Among the most well-documented examples is methicillin-resistant Staphylococcus aureus (MRSA), long associated with substantial mortality worldwide [11]. Equally concerning are drug-resistant tuberculosis strains; currently, 3.5% of newly diagnosed TB cases and 18% of previously treated TB cases are multidrug-resistant (MDR-TB), while reports of extensively drug-resistant TB (XDR-TB) are on the rise [12].
While antibiotics remain indispensable in clinical practice, decades of overuse, under-dosing, and inappropriate treatment duration have accelerated the development of resistance. Moreover, the non-scientific and unregulated application of antimicrobials in livestock feed, particularly in developing countries, has significantly contributed to the spread of resistant bacteria [13]. The consequences of antibiotic resistance extend beyond therapeutic failures. On the preventive side, AMR jeopardizes the safety of complex medical interventions, including cancer chemotherapy, organ transplantation, and invasive procedures such as intubation or catheterization, all of which rely heavily on effective prophylaxis against infections [14,15].
Unfortunately, the global research pipeline for new antibiotics has failed to keep pace with the growing threat. Pharmaceutical industries began retreating from antibiotic development in the 1980s, largely due to high costs, low profitability, and complex regulatory challenges. The last major broad-spectrum antibiotic class—fluoroquinolones—was discovered in the 1980s and commercialized in 1987. Since then, innovation has slowed dramatically, with only a handful of new agents emerging [16]. Given that antibiotic usage itself accelerates resistance, reducing unnecessary prescriptions is one of the most effective strategies to delay resistance. At the same time, it is vital to safeguard the efficacy of existing antimicrobials, as no significant breakthrough molecules have been discovered in recent decades [17]. This narrative review therefore focuses on the underlying mechanisms of microbial resistance, the factors fueling AMR, and the essential strategies that must be prioritized to counter this escalating global health crisis.
TIMELINE OF MAJOR ANTIBIOTIC DISCOVERIES AND THE EMERGENCE OF RESISTANCE
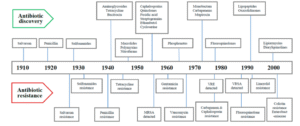
The onset of the modern antibiotic era is often traced back to 1910 with the synthesis of salvarsan and neosalvarsan by Paul Ehrlich, which were used to treat syphilis caused by Treponema pallidum. Subsequently, prontosil, a sulfonamide prodrug discovered by bacteriologist Gerhard Domagk, gradually supplanted salvarsan in clinical use. In the 1930s, American microbiologist and biochemist Selman Waksman pioneered the systematic screening of soil microbes for bioactive compounds, ultimately identifying numerous antibiotics from filamentous actinomycetes, including streptomycin, a cornerstone in tuberculosis treatment. Waksman also formalized the definition of an antibiotic as “a compound produced by a microorganism to inhibit or destroy other microbes.”
The discovery of penicillin from Penicillium rubens by Scottish physician Alexander Fleming in 1928 marked the beginning of the so-called golden era of antibiotics, which reached its peak in the mid-1950s. The period from the 1940s to 1960s is widely regarded as the “Golden Age” of antibiotic discovery, during which most of the drugs still in clinical use today were developed. Following this period, antibiotic innovation gradually declined, while concurrently, the emergence of drug-resistant pathogens became increasingly apparent [16]. Indeed, resistance has been observed almost simultaneously with the advent of each new antibiotic. Even before penicillin was introduced therapeutically in 1940, the first penicillin-resistant Staphylococcus strain had already been documented. Methicillin, the first semisynthetic penicillin designed to resist penicillinase, was launched in 1959, yet a methicillin-resistant Staphylococcus strain was reported just one year later, in 1960 [18]. Similarly, vancomycin, a glycopeptide introduced in 1958 as a last-resort treatment for methicillin-resistant staphylococcal infections, saw the emergence of vancomycin-resistant coagulase-negative staphylococci (CoNS) in 1979. By the late 1980s, vancomycin-resistant Enterococcus (VRE) was documented, and vancomycin efficacy against Staphylococcus aureus began to decline, with vancomycin-intermediate S. aureus (VISA) and vancomycin-resistant S. aureus (VRSA) reported in 1997 and 2002, respectively [19].
Cephalosporins, a class of β-lactam antibiotics, were discovered in 1945 and introduced clinically in 1964 to treat penicillin-resistant infections. Multiple generations have since been developed, with the fifth generation now available. Initially highly effective, particularly against extended-spectrum β-lactamase (ESBL)-producing Gram-negative bacteria, resistance has developed across earlier generations, including the fourth. Tetracycline, discovered in 1950, was widely used for common bacterial infections, including gastrointestinal illnesses, but within a decade, Shigella strains exhibited resistance by 1959. The fluoroquinolone levofloxacin, a third-generation antibiotic, was introduced in 1996, yet levofloxacin-resistant Pneumococcus was reported in the same year [20]. Carbapenems, another class of β-lactams introduced in 1980, were reserved for treatment of infections caused by Enterobacterales, especially cephalosporin-resistant strains. However, with increasing use in the 1990s and 2000s, carbapenem-resistant Enterobacterales (CRE) emerged in multiple countries from 2006 onward [21]. Reviewing the timeline of antibiotic development, it is clear that pharmaceutical innovation in novel antibiotic classes primarily occurred between 1960 and 1980. Since then, the pace of discovery has markedly slowed, creating a substantial mismatch between the rising prevalence of drug-resistant pathogens and the availability of effective antibiotics [17]. This imbalance has fueled concerns among experts about the possibility of a post-antibiotic era. Figure 1 illustrates the timeline of major antibiotic discoveries alongside the emergence of corresponding resistance patterns.
-
SUPERBUGS
The term superbugs describe microorganisms that have developed resistance to multiple antimicrobial agents used for their treatment, encompassing both multidrug-resistant and pan-drug-resistant bacteria and fungi. Infections caused by superbugs are often extremely difficult—or sometimes impossible—to treat with currently available therapeutics. The acronym “ESKAPE” represents six of the most notorious drug-resistant bacteria: Enterobacterales, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter. Presently, globally prevalent superbugs include carbapenem-resistant Enterobacterales (CRE), carbapenem-resistant Klebsiella pneumoniae (CRKP), methicillin-resistant Staphylococcus aureus (MRSA), ESBL-producing Enterobacterales, vancomycin-resistant Enterococcus (VRE), multidrug-resistant Pseudomonas aeruginosa, and multidrug-resistant Acinetobacter. The emergence of multidrug-resistant bacteria is closely linked to the prolonged and extensive use of antibiotics. For instance, Mycobacterium tuberculosis has evolved into MDR-TB after decades of antitubercular treatment, and it remains a major superbug in both developing and underdeveloped regions. Hospital-acquired infections (HAIs), caused by both Gram-positive bacteria (Staphylococcus epidermidis, Clostridioides difficile, Streptococcus pneumoniae) and Gram-negative bacteria (Burkholderia cepacia, Stenotrophomonas maltophilia, Campylobacter jejuni, Citrobacter freundii, Enterobacter spp., Haemophilus influenzae, Proteus mirabilis, Salmonella spp., and Serratia spp.), are frequently classified as superbugs due to the lack of effective antibiotics to treat them [22]. Infections with superbugs significantly elevate morbidity and mortality rates, as available therapeutic options are severely limited, while treatment costs and hospital stays are markedly increased [23].
-
BASIS OF ANTIBIOTIC RESISTANCE
Antibiotic resistance represents an evolutionary adaptation of bacteria to survive exposure to antimicrobial agents. Clinically, pathogens are initially susceptible when an antibiotic is introduced, but with repeated exposure, bacteria develop resistance. From an evolutionary standpoint, resistance arises either through chromosomal mutations or the acquisition of foreign genetic material via horizontal gene transfer (HGT), which carries resistance determinants. Mutations typically target three types of genes: those encoding antibiotic targets, transport proteins involved in drug influx/efflux, and regulators that control expression of efflux pumps or antibiotic-modifying enzymes, thereby enabling resistance. Evidence suggests that commensal or environmental bacteria act as reservoirs of resistance genes, which are subsequently transferred to pathogenic bacteria through HGT [24]. Many antibiotics are naturally produced by environmental microorganisms. To prevent self-toxicity, these organisms inherently possess resistance genes, allowing them to survive their own antibiotic production [25]. Resistance in bacteria can arise from intrinsic, acquired, or adaptive mechanisms [26].
Intrinsic resistance refers to the inherent ability of bacteria to resist specific classes of antibiotics due to naturally occurring chromosomal genes, without requiring mutations or external gene acquisition. This form of resistance often involves efflux pumps and reduced membrane permeability, and may affect multidrug efflux systems [27,28]. Acquired resistance occurs when previously susceptible bacteria gain resistance through chromosomal mutations or the uptake of exogenous genes via HGT. HGT can occur through transformation, transposition, or conjugation, with plasmid-mediated conjugation being the most common. Acquired resistance can be either temporary or permanent, depending on the genetic context [29,30]. Adaptive resistance is a conditional, environmentally induced phenotype that may be transient or persistent depending on selection pressures. Exposure to subinhibitory concentrations of antibiotics, along with environmental cues such as nutrient availability, stress, pH, and ion concentrations, can induce adaptive resistance in bacteria found in humans and livestock. Unlike intrinsic and acquired resistance, adaptive resistance generally reverts to the original phenotype when the inducing conditions are removed. Although the underlying biological mechanisms remain incompletely understood, factors such as high mutation rates, gene amplification, efflux pumps, biofilm formation, epigenetic inheritance, population heterogeneity, and microbial community structure have been implicated in its development [31,32].
-
SOURCES AND ROUTES OF TRANSMISSION OF AMR
The spread and acquisition of antimicrobial resistance (AMR) primarily occur through human-to-human interactions, both within healthcare settings and in the community. Various reservoirs—including humans, animals, water, and the broader environment—harbor antimicrobial-resistant genes, which can transfer between and within these reservoirs. Transmission patterns vary significantly depending on the bacterial species and the specific resistance determinants involved [33]. Certain hotspot sources significantly facilitate the dissemination of resistant bacteria, such as wastewater and sludge from urban treatment plants, and natural fertilizers including pig slurry, cow manure, and poultry-derived fertilizers [34]. Another direct route involves the use of antibiotic-treated animal feeds, with resistant bacteria subsequently transmitted to humans through the consumption of these animals [35]. Additional transmission pathways include ingestion of fecal-contaminated food or water and direct human-animal contact, which further promote the movement of resistance genes across species [36].
-
MECHANISMS OF DRUG RESISTANCE
In natural ecosystems, antimicrobials and bacteria coexist, and bacteria have evolved various strategies to counteract the inhibitory effects of antibiotic molecules. Antibiotics primarily target four essential bacterial components: the cell wall, cell membrane, protein synthesis machinery, and nucleic acid synthesis. The primary mechanisms by which bacteria acquire resistance include: reducing drug uptake, modifying drug targets, inactivating the drug, and enhancing active drug efflux (Figure 2). Intrinsic resistance mechanisms often rely on restricted drug entry, enzymatic drug inactivation, and efflux pumps. Structural differences between Gram-positive and Gram-negative bacteria contribute to variations in their resistance strategies. Gram-positive bacteria, lacking an outer lipopolysaccharide (LPS) membrane, rely less on restricting drug uptake and have a limited capacity for efflux of certain antibiotics [37,38]. In contrast, Gram-negative bacteria employ all four primary resistance mechanisms, including limiting uptake, modifying targets, drug inactivation, and active efflux, making them particularly adept at surviving in the presence of diverse antibiotics.
6.1. Limiting Drug Uptake
In Gram-negative bacteria, lipopolysaccharide (LPS), a highly acylated glycolipid, constitutes a major part of the outer membrane and acts as a permeability barrier to numerous compounds, including antibiotics. This intrinsic feature reduces the entry of certain antibiotics, contributing to natural resistance. Additionally, alterations in outer-membrane proteins, particularly porins, can result in acquired resistance. Porins function as primary channels for hydrophilic antibiotics such as β-lactams, fluoroquinolones, tetracyclines, and chloramphenicol. The number and type of porin proteins influence antibiotic uptake, directly affecting bacterial susceptibility [39]. Acquired resistance can also arise from mutations that reduce porin expression or impair their function. When these mutations coincide with other resistance mechanisms—such as efflux pumps or enzymatic antibiotic degradation—they can confer high-level resistance [40]. Another important mechanism is biofilm formation by bacteria including Enterococcus faecalis, Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus viridans, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, and Pseudomonas aeruginosa. Biofilms are structured communities of microbial cells embedded in self-produced exopolysaccharide matrices attached to biotic or abiotic surfaces. Biofilms confer enhanced tolerance and resistance to antibiotics by obstructing drug penetration and preventing the maintenance of bactericidal concentrations throughout the microbial community [41,42].
6.2. Modification of Targets for Drug
Bacteria can evade antibiotics by modifying the drug’s target, thereby preventing effective binding. These modifications typically arise from spontaneous mutations in genes encoding the target proteins. For example, mutations in the quinolone-resistance-determining region (QRDR) of DNA gyrase (topoisomerase II and IV) result in fluoroquinolone resistance in both Gram-positive and Gram-negative bacteria [43]. Methylation represents another efficient strategy for target modification. Methylases such as erm genes confer resistance to macrolides, lincosamides, and streptogramin B antibiotics across Gram-positive and Gram-negative species. Similarly, methylation of the cfr gene has been associated with resistance in multiple bacterial genera, including Proteus vulgaris, Staphylococcus spp., Enterococcus spp., Bacillus spp., and E. coli [44]. In Staphylococcus spp., resistance to β-lactam antibiotics is significantly enhanced by the expression of alternative penicillin-binding proteins, encoded by the mecA and mecC genes, which reduce the drug’s binding affinity [45,46].
6.3. Inactivation of Drug
Bacteria can acquire antibiotic resistance by inactivating drugs, which occurs through two main mechanisms: either the antibiotic molecule is chemically degraded, or a functional chemical group is transferred onto it. A well-known example involves β-lactamases, hydrolyzing enzymes produced by members of the Enterobacterales family, which effectively inactivate β-lactam antibiotics. Initially referred to as penicillinases and cephalosporinases, these enzymes open the β-lactam ring, preventing the antibiotic from binding to its target, the penicillin-binding proteins. Many Enterobacterales species, as well as Gram-positive bacteria like Staphylococcus aureus, Enterococcus faecalis, and Enterococcus faecium, carry β-lactamase genes, often transmitted via horizontal gene transfer (HGT). Similarly, tetracycline inactivation occurs through hydrolysis mediated by an enzyme encoded by the tetX gene in certain bacterial strains [47]. Other common chemical modifications for drug inactivation include acetylation, phosphorylation, and adenylation. Phosphorylation and adenylation are frequently employed against aminoglycosides, while acetylation is a versatile mechanism acting on aminoglycosides, chloramphenicol, streptogramins, and fluoroquinolones [38].
6.4. Efflux of Drug
Bacteria use energy-dependent efflux pumps located in the cytoplasmic membrane to regulate the intracellular concentration of antibiotics and other toxic compounds. By actively expelling harmful agents, including antibiotics, metabolic byproducts, and quorum-sensing molecules, efflux pumps help bacteria maintain homeostasis. The first plasmid-encoded efflux pump was described in Escherichia coli in 1980, which transported tetracycline out of the cell. Since then, a wide range of Gram-positive and Gram-negative bacteria with diverse efflux mechanisms have been identified. Most efflux systems are multidrug pumps that are chromosomally encoded, contributing to intrinsic bacterial resistance [48]. In contrast, substrate-specific pumps targeting antibiotics like chloramphenicol, tetracyclines, and macrolides are often carried on mobile genetic elements [38,49]. Based on structure and energy source, six major families of efflux pumps exist: ATP-binding cassette (ABC) superfamily, major facilitator superfamily (MFS), multidrug and toxic compound extrusion (MATE) family, small multidrug resistance (SMR) family, resistance–nodulation–division (RND) superfamily, and drug/metabolite transporter (DMT) superfamily. In Gram-positive bacteria, most efflux pumps belong to the ABC and MFS families, encoded either chromosomally or on plasmids. Conversely, in Gram-negative bacteria, the clinically significant pumps are primarily members of the RND superfamily, composed of an outer-membrane channel, a periplasmic adaptor, and a cytoplasmic membrane pump [50].
-
DRIVERS OF AMR
Antimicrobial resistance (AMR) is driven by a complex interplay of microbial traits and environmental factors, encompassing behaviors of both prescribers and consumers. Broadly, the factors contributing to AMR can be classified into four categories: environmental factors (e.g., overcrowded populations, rapid transmission through travel, poor sanitation, ineffective infection control programs, and extensive agricultural antibiotic use), drug-related factors (e.g., counterfeit or substandard medications, and over-the-counter availability), patient-related factors (e.g., poor compliance, poverty, lack of education, self-medication, and misconceptions), and physician-related factors (e.g., inappropriate prescription, inadequate dosing, and lack of updated training) [38,51]. The major AMR-driving factors are elaborated below.
7.1. Misuse and Overuse of Antibiotics
Although antibiotic resistance naturally occurs as part of microbial evolution, its rate has been significantly accelerated by misuse in humans and animals. Epidemiological studies reveal a causal relationship between overuse and the emergence of resistance [52]. Despite repeated warnings from health organizations, antibiotic misuse continues at alarming levels worldwide, with the current scenario approaching a critical tipping point. Global surveys indicate that misconceptions about antibiotics are widespread, particularly among less-educated populations, including the belief that antibiotics are effective against common viral infections such as colds or flu. In many developing countries, antibiotics are overprescribed, partly due to inadequate diagnostic facilities [53]. Examples of misuse include administering antibiotics without proper indication. The unregulated over-the-counter availability of antibiotics for both humans and animals further accelerates resistance. Lack of national antibiotic policies and standard treatment guidelines exacerbates the problem, while substandard or poor-quality antibiotics in supply chains worsen AMR in several developing nations. Additionally, physicians may prescribe prolonged courses or inappropriate doses, sometimes influenced by financial incentives or patient expectations [53,54].
7.2. Increase in Gross Domestic Product (GDP)
The global rise in antibiotic use has been closely linked to increases in GDP, particularly in developing countries. Economic growth has improved living standards in low- and middle-income countries, which correlates with higher consumption of antibiotics. Between 2000 and 2015, global antibiotic use rose by approximately 65% [55]. Alongside this, greater consumption of animal protein has contributed to the transmission of AMR from animal sources in these countries [56].
7.3. Inappropriate Prescribing Patterns
Improper prescription practices are a major driver of AMR [57]. This includes prescribing antibiotics unnecessarily, selecting the wrong antibiotic, or using incorrect doses and durations [58]. Studies have shown that at least 50% of hospital patients receive antibiotics without compelling clinical indications. Ideally, antibiotic therapy should be guided by isolation and antimicrobial susceptibility testing, yet a CDC report (2017) found that roughly one-third of hospital patients received antibiotics without proper testing, often continued for excessive durations [59]. Nursing homes display even higher rates of misprescription, with approximately 75% of antibiotics prescribed incorrectly in terms of drug, dose, or duration [60].
7.4. Paucity of Futuristic Antibiotics
The growing threat of antibiotic resistance underscores the urgent need for novel drug development [61]. Unfortunately, despite repeated calls from the WHO, the pharmaceutical pipeline remains sparse. Of 51 newly developed antibiotics, only 8 are truly innovative, with the majority being reformulations of older drugs. Consequently, resistance may emerge rapidly against these new agents. The limited availability of new drugs has seriously compromised treatment of drug-resistant TB, urinary tract infections, pneumonia, and Gram-negative infections, leaving vulnerable populations, such as the very young and elderly, at heightened risk [62]. Regulatory constraints and economic considerations are major barriers to antibiotic innovation. Many pharmaceutical companies have reduced investments in antibiotic R&D, and 18 major firms have abandoned production entirely. Prioritizing profitability, pharma companies have shifted focus to drugs for chronic diseases rather than infectious diseases, further limiting the development of lifesaving antibiotics.
7.5. Agricultural Use of Antibiotics
The use of antibiotics in livestock farming has increased substantially in many developing countries, largely driven by the growing demand for animal protein. This practice contributes to the rise of AMR due to residues of antibiotics in animal-derived products, such as muscles, kidney, liver, fat, milk, and eggs. Antibiotics are commonly applied for various purposes, including treating animal illnesses, supplementing feed to promote growth, enhancing feed conversion efficiency, and disease prevention [63]. The widespread and often unregulated use of antibiotics in food animal production, particularly in developing countries seeking higher farm incomes and lacking strict government policies, has become a significant contributor to human AMR [64]. In the United States, approximately 70% of medically important antibiotics are sold for use in animals [65]. A major concern is that antibiotics used in veterinary practice often share types, mechanisms of action, or classes with human-prescribed antibiotics, raising the risk of cross-resistance.
7.6. Easy Travel Routes
The global spread of antibiotic-resistant bacteria is increasingly facilitated by human mobility. Modern travel, including the movement of humans, animals, and goods, contributes significantly to the dissemination of AMR worldwide [66]. Travelers to regions with high endemicity of resistant pathogens may unknowingly carry antimicrobial-resistant organisms back to their home countries. Studies show that such bacteria can persist in the human body for up to 12 months after travel, creating a prolonged window for transmission to susceptible populations [67].
7.7. Knowledge Gap
Evidence indicates that both healthcare workers (HCWs) and the general public have substantial gaps in knowledge regarding appropriate antibiotic use and the mechanisms driving antibiotic resistance [68]. Effective surveillance is essential to quantify the burden of AMR and design targeted intervention strategies, such as antimicrobial stewardship programs. However, comprehensive statistical data on antibiotic consumption and AMR prevalence in both healthcare and agricultural sectors remain lacking worldwide [69]. Surveillance data are critical for identifying priority areas for intervention and guiding cooperative efforts across international agencies, human and veterinary medicine, agriculture, animal production industries, and consumers. Addressing this knowledge gap is a prerequisite for launching effective AMR containment strategies.
-
Clinical Implications of AMR
Antimicrobial resistance has significant clinical implications that threaten the effective management of infectious diseases [70]. Successful treatment of microbial infections, including bacterial, fungal, and viral infections, is increasingly hindered by the emergence of resistant pathogens. The development and dissemination of new resistance mechanisms jeopardize the treatment of common illnesses such as urinary tract infections, upper respiratory tract infections, typhoid, and influenza, often resulting in treatment failure, permanent disability, or even death. Furthermore, the effectiveness of critical medical interventions, including cancer chemotherapy, transplantation surgeries, and even minor dental procedures, is compromised in the absence of novel antimicrobial drugs. Infections caused by resistant microorganisms frequently require prolonged therapy with higher healthcare costs and may necessitate the use of expensive alternative drugs, further straining healthcare systems and patient resources.
-
How to Combat AMR
Antimicrobial resistance is a pressing concern that affects not only humans but also animals, plants, and the broader environment. Animals can serve as potential reservoirs of multidrug-resistant (MDR) pathogens, which may be transmitted to humans through direct contact or the consumption of animal-derived foods. Addressing AMR is not a challenge that can be managed by a single government department or independent organization; it requires coordinated efforts and collaboration across multiple sectors, including healthcare industries, pharmacy, agriculture, finance, trade, education, and non-governmental organizations at both national and international levels. Multisectoral collaboration can operate horizontally, across sectors and departments within a country through multistakeholder forums, and vertically, across different administrative levels within a country, a region, or internationally [71]. One of the key measures to combat AMR includes curbing the inappropriate prescription of broad-spectrum antibiotics for trivial conditions, alongside careful monitoring of antimicrobial use in animals by veterinarians. Rational antibiotic prescription, limited prophylactic use of antimicrobials, patient education, compliance with therapy, and proper hospital hygiene via antimicrobial stewardship programs are among the main interventions [72]. The development and deployment of rapid diagnostic tools and precise antimicrobial profiling for targeted therapy are also essential components.
The World Health Assembly has adopted five strategic action plans to combat AMR: (1) improving awareness and understanding of antimicrobial resistance, (2) strengthening knowledge through surveillance and research in infection control, (3) implementing effective sanitation, hygiene, and infection prevention measures, (4) optimizing antimicrobial use in both human and animal health, and (5) encouraging sustainable investment in new medicines, diagnostic tools, and vaccines [73]. On an international scale, measures include establishing and strengthening collaborations among agencies, governments, NGOs, and professional groups; creating global surveillance networks for antimicrobial use and AMR; enhancing laboratory capacity for detecting and reporting AMR pathogens; developing international tracking systems for early identification and mitigation of emerging pathogens; monitoring and controlling counterfeit antimicrobials worldwide; and investing in research, drug discovery, and vaccine development. At the national level, strategies involve implementing comprehensive antibiotic policies for judicious use in healthcare and agricultural settings, strengthening surveillance and monitoring through integration of public health and veterinary sectors, developing innovative point-of-care diagnostic tests for pathogen detection and resistance monitoring, investing in research on new antibiotics and vaccines, building capacity and fostering international collaboration, and adopting antimicrobial stewardship programs aligned with essential drug lists [69].
Rational use of antibiotics is essential to minimize the development of antimicrobial resistance. The World Health Organization (WHO) defines the rational use of medicine as using appropriate medications, including antibiotics, tailored to patients’ clinical needs, at correct doses, for adequate durations, and at the lowest possible cost [70]. Optimal outcomes in infection treatment can only be achieved when pathogen selection, drug toxicity, and resistance development are minimized through rational antibiotic use. Antibiotic stewardship programs (ASPs) in healthcare settings are primarily aimed at ensuring such rational use. In parallel, stringent regulatory control over over-the-counter (OTC) sales of oral and injectable antibiotics must be enforced, as uncontrolled access remains common in many underdeveloped and developing countries. Antibiotics should only be dispensed upon prescription by qualified physicians, accompanied by ongoing awareness programs for both patients and pharmacy personnel, and continuous reappraisal of local antibiotic policies based on regional AMR surveillance data [74].
Infection prevention and control (IPC) is another cornerstone in combating AMR, as it protects both patients and healthcare workers from avoidable infections, including those caused by drug-resistant pathogens. Physicians, nurses, pharmacists, and other healthcare providers play pivotal roles in IPC, including compliance with hospital infection control and antibiotic policies, timely reporting of resistant cases, and educating patients on treatment compliance [75]. Recommended IPC measures in healthcare facilities include forming infection prevention committees, practicing good hand hygiene, accurate diagnosis and treatment, responsible antimicrobial use, continuous surveillance of antibiotic use and resistance, ensuring a quality antimicrobial supply chain, and maintaining good microbiological laboratory practices. Antimicrobial stewardship programs further support these measures by guiding prescribers on proper antibiotic selection, dosage, and duration, reducing overuse and misuse, and minimizing resistance development. The CDC’s “Core Elements” for antimicrobial stewardship provide structured guidance applicable to hospitals of all sizes [76,77].
The use of antibiotics in animals also demands regulation, as the WHO emphasizes strict legislation on medically important antibiotics to limit their use for growth promotion and disease prevention, advocating alternative measures such as improved hygiene, probiotics, vaccination, and optimized husbandry practices [78]. Research and development of new drugs and vaccines are vital to stay ahead of rapidly evolving resistance, with vaccines reducing antimicrobial demand and posing no risk for resistance development. Novel vaccines against drug-resistant pathogens, including carbapenem-resistant Enterobacterales and Acinetobacter baumannii, are especially important [73,75].
Additional measures include establishing checkpoints to prevent illegal sales and self-medication of antibiotics, especially in low-income countries, and introducing strategies such as delayed antibiotic prescribing where appropriate [58,60]. Community engagement is critical, as local practices related to hygiene, food production, health-seeking behavior, and waste disposal influence AMR. Behavioral change programs tailored to communities can help safeguard treatment options and reduce AMR propagation [79].
Alternatives to antibiotics are being explored, including natural compounds from plants such as polyphenolics, alkaloids, and flavonoids, though many remain in preclinical stages [80–86]. Advanced biotechnological approaches offer opportunities to harness microbial interactions for discovering new antimicrobial therapies [87]. Phage therapy, employing bacteriophages to target pathogenic bacteria, shows promise due to its specificity, autodosing, and low toxicity, though challenges such as phage selection and immune responses must be addressed [88]. Antivirulence drugs represent another strategy, disarming bacteria by targeting virulence factors without promoting resistance or disturbing microbiota, with some FDA-approved applications and promising results against MRSA in animal studies [89]. Bacteriocins, natural antimicrobial peptides, are increasingly explored for both clinical and food preservation applications, with nisin showing activity against multiple drug-resistant pathogens including MRSA, Streptococcus pneumoniae, Enterococci, Clostridioides difficile, and Enterobacterales [79].
The One Health approach integrates human, animal, and environmental health to combat AMR through communication, coordination, and collaboration. Established in 2008 by WHO in partnership with the FAO and OIE, One Health promotes multisectoral strategies for surveillance, evidence-based interventions, and policy implementation. Key stakeholders include healthcare professionals, veterinarians, ecologists, and agricultural workers, all collaborating to monitor, prevent, and control AMR across domains [90,91]. Advanced tools such as whole-genome sequencing (WGS) and next-generation sequencing (NGS) further support surveillance and research under the One Health framework, helping to guide targeted interventions and optimize outcomes.
-
CONCLUSIONS
The evolution of antimicrobial resistance (AMR) in bacteria is a continuous process occurring either through new chromosomal mutations or the acquisition of drug-resistance genes via horizontal gene transfer (HGT). Over the past two decades, the incremental development of AMR has emerged as a serious global public health threat, now recognized as one of the highest health dangers of the 21st century, severely limiting treatment options. Multidrug-resistant (MDR) bacteria are frequently implicated in common infections, including respiratory, urinary, sexually transmitted, and tuberculosis infections worldwide. Meanwhile, the development and supply of new antibiotics have lagged significantly since the 1980s and are not keeping pace with the rapid emergence of resistant pathogens. In this context, the future of successful antimicrobial therapy appears bleak, and without coordinated global action, the prospect of a postantibiotic era is more plausible than a hypothetical scenario. Multiple drivers contribute to the global emergence and dissemination of AMR, posing a significant concern for both human and animal health. Infections caused by antimicrobial-resistant organisms are more difficult to treat, resulting in higher rates of treatment failure, complications, prolonged hospital stays, and substantial economic costs for individuals and society. Prudent and rational use of antibiotics—including appropriate dosage and duration—remains among the most effective strategies to reduce selective pressure and curb the emergence of resistance. Equally critical is the strict implementation of infection prevention and control measures in all healthcare facilities, which is vital for containing the spread of MDR organisms [57,58].
Combating AMR requires a coordinated and sustained global effort involving international governmental and nongovernmental agencies, underpinned by strong political commitment. Integration and collaboration among policymakers, researchers, public health practitioners, pharmaceutical companies, hospital administrators, agricultural industry leaders, and the general public are essential. The overarching goal of this collaboration is to slow the progression of AMR and mitigate its health and economic burdens. Key strategies include the establishment of antimicrobial stewardship programs, strict adherence to antibiotic policies in healthcare settings, good microbiology practices, surveillance and monitoring of resistance patterns, minimizing over-the-counter antibiotic use and use in food animals, and ensuring access to quality and affordable medicines, vaccines, and diagnostics [73,75–78]. Prevention remains the most effective approach to reduce antimicrobial-resistant infections and their transmission. While the rational use of existing antibiotics is essential to restore their efficacy, urgent efforts must focus on the development of new antibiotics, alternative therapies, and innovative technologies in diagnostics and vaccine development. Despite numerous initiatives to address antibiotic resistance, coordinated global action, particularly political will at national and international levels, remains insufficient. The persistent rise of antimicrobial-resistant infections indicates that, without immediate intervention, we may soon face severe setbacks in medical, social, and economic sectors, potentially undermining critical achievements in modern medicine, including major surgeries, organ transplantation, care of preterm infants, and cancer chemotherapy.
Author Contributions
Conceptualization, E.J.C.; Literature review, E.J.C.; Methodology, M.R.T.; Data curation, M.R.T.; Supervision, L.S.M.; Validation and editing, L.S.M. All authors have read and agreed to the published version of the manuscript.
Acknowledgments:
The authors gratefully acknowledge the support of the University of Cambridge, Department of Microbiology and Immunology, for academic and technical assistance.
Funding: This study did not receive financial support from any funding agency, whether public, private, or non-profit.
Conflict of Interest: The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- Williams-Nguyen, J.; Sallach, J.B.; Bartelt-Hunt, S.; Boxall, A.B.; Durso, L.M.; McLain, J.E.; Singer, R.S.; Snow, D.D.; Zilles, J.L. Antibiotics and Antibiotic Resistance in Agroecosystems: State of the Science. J. Environ. Qual. 2016, 45, 394–406. [CrossRef]
- How Antimicrobial Resistance Happens. Available online: https://www.cdc.gov/drugresistance/about/how-resistancehappens.html (accessed on 2 June 2023).
- Tenover, F.C. Mechanisms of antimicrobial resistance in bacteria. Am. J. Med. 2006, 119, S3–S10; discussion S62–S70. [CrossRef]
- Zhou, G.; Shi, Q.S.; Huang, X.M.; Xie, X.B. The Three Bacterial Lines of Defense against Antimicrobial Agents. Int. J. Mol. Sci. 2015, 16, 21711–21733. [CrossRef] [PubMed]
- Khameneh, B.; Diab, R.; Ghazvini, K.; Fazly Bazzaz, B.S. Breakthroughs in bacterial resistance mechanisms and the potential ways to combat them. Microb. Pathog. 2016, 95, 32–42. [CrossRef]
- Read, A.F.; Woods, R.J. Antibiotic resistance management. Evol. Med. Public Health 2014, 2014, 147. [CrossRef] [PubMed]
- George, A. Antimicrobial resistance, trade, food safety and security. One Health 2018, 5, 6–8. [CrossRef]
- Samreen; Ahmad, I.; Malak, H.A.; Abulreesh, H.H. Environmental antimicrobial resistance and its drivers: A potential threat to public health. J. Glob. Antimicrob. Resist. 2021, 27, 101–111. [CrossRef]
- Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [CrossRef] [PubMed]
- O’Neill, J. Antimicrobial resistance: Tackling a crisis for the health and wealth of nations (The Review on Antimicrobial Resistance, London, 2016, United Kingdom). Rev. Antimicrob. Resist. 2014.
- Antimicrobial Resistance. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobialresistance (accessed on 2 November 2022).
- Multidrug-Resistant Tuberculosis (MDR-TB). Available online: https://www.who.int/docs/default-source/documents/ tuberculosis/multidrug-resistant-tuberculosis-mdr-tb.pdf (accessed on 4 June 2023)
- Ghimpet,eanu, O.M.; Pogurschi, E.N.; Popa, D.C.; Dragomir, N.; Drăgotoiu, T.; Mihai, O.D.; Petcu, C.D. Antibiotic Use in Livestock and Residues in Food-A Public Health Threat: A Review. Foods 2022, 11, 1430. [CrossRef]
- Founou, R.C.; Founou, L.L.; Essack, S.Y. Clinical and economic impact of antibiotic resistance in developing countries: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0189621. [CrossRef] [PubMed]
- Levy, S.B.; Marshall, B. Antibacterial resistance worldwide: Causes, challenges and responses. Nat. Med. 2004, 10, S122–S129. [CrossRef] [PubMed]
- Hutchings, M.I.; Truman, A.W.; Wilkinson, B. Antibiotics: Past, present and future. Curr. Opin. Microbiol. 2019, 51, 72–80. [CrossRef] [PubMed]
- Iskandar, K.; Murugaiyan, J.; Hammoudi Halat, D.; Hage, S.E.; Chibabhai, V.; Adukkadukkam, S.; Roques, C.; Molinier, L.; Salameh, P.; Van Dongen, M. Antibiotic Discovery and Resistance: The Chase and the Race. Antibiotics 2022, 11, 182. [CrossRef]
- Uddin, T.M.; Chakraborty, A.J.; Khusro, A.; Zidan, B.R.M.; Mitra, S.; Emran, T.B.; Dhama, K.; Ripon, M.K.H.; Gajdács, M.; Sahibzada, M.U.K.; et al. Antibiotic resistance in microbes: History, mechanisms, therapeutic strategies and future prospects. J. Infect. Public Health 2021, 14, 1750–1766. [CrossRef]
- Parmar, A.; Lakshminarayanan, R.; Iyer, A.; Mayandi, V.; Leng Goh, E.T.; Lloyd, D.G.; Chalasani, M.L.S.; Verma, N.K.; Prior, S.H.; Beuerman, R.W.; et al. Design and Syntheses of Highly Potent Teixobactin Analogues against Staphylococcus aureus, Methicillin-Resistant Staphylococcus aureus (MRSA), and Vancomycin-Resistant Enterococci (VRE) in Vitro and in Vivo. J. Med. Chem. 2018, 61, 2009–2017. [CrossRef]
- Zaman, S.B.; Hussain, M.A.; Nye, R.; Mehta, V.; Mamun, K.T.; Hossain, N. A Review on Antibiotic Resistance: Alarm Bells are Ringing. Cureus 2017, 9, e1403. [CrossRef]
- Suay-García, B.; Pérez-Gracia, M.T. Present and Future of Carbapenem-resistant Enterobacteriaceae (CRE) Infections. Antibiotics 2019, 8, 122. [CrossRef]
- Kaur, N.; Prasad, R.; Varma, A. Prevalence and antibiotic susceptibility pattern of methicillin resistant staphylococcus aureus in tertiary care hospitals. Biotechnol. J. Int. 2014, 4, 228–235. [CrossRef]
- Parmanik, A.; Das, S.; Kar, B.; Bose, A.; Dwivedi, G.R.; Pandey, M.M. Current Treatment Strategies Against Multidrug-Resistant Bacteria: A Review. Curr. Microbiol. 2022, 79, 388. [CrossRef]
- Davies, J.; Davies, D. Origins and evolution of antibiotic resistance. Microbiol. Mol. Biol. Rev. MMBR 2010, 74, 417–433. [CrossRef] [PubMed]
- Koch, N.; Islam, N.F.; Sonowal, S.; Prasad, R.; Sarma, H. Environmental antibiotics and resistance genes as emerging contaminants: Methods of detection and bioremediation. Curr. Res. Microb. Sci. 2021, 2, 100027. [CrossRef]
- Lee, J.H. Perspectives towards antibiotic resistance: From molecules to population. J. Microbiol. 2019, 57, 181–184. [CrossRef] [PubMed]
- Martinez, J.L. General principles of antibiotic resistance in bacteria. Drug Discov. Today. Technol. 2014, 11, 33–39. [CrossRef] [PubMed]
- Cox, G.; Wright, G.D. Intrinsic antibiotic resistance: Mechanisms, origins, challenges and solutions. Int. J. Med. Microbiol. IJMM 2013, 303, 287–292. [CrossRef] [PubMed]
- Holmes, A.H.; Moore, L.S.; Sundsfjord, A.; Steinbakk, M.; Regmi, S.; Karkey, A.; Guerin, P.J.; Piddock, L.J. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet 2016, 387, 176–187. [CrossRef]
- Munita, J.M.; Arias, C.A. Mechanisms of Antibiotic Resistance. Microbiol. Spectr. 2016, 4. [CrossRef]
- Fernández, L.; Hancock, R.E. Adaptive and mutational resistance: Role of porins and efflux pumps in drug resistance. Clin. Microbiol. Rev. 2012, 25, 661–681. [CrossRef]
- Rizi, K.S.; Ghazvini, K.; Noghondar, M.K. Adaptive antibiotic resistance: Overview and perspectives. J. Infect. Dis. Ther. 2018, 6, 363. [CrossRef]
- Godijk, N.G.; Bootsma, M.C.J.; Bonten, M.J.M. Transmission routes of antibiotic resistant bacteria: A systematic review. BMC Infect. Dis. 2022, 22, 482. [CrossRef]
- Krzemi ´nski, P.; Markiewicz, Z.; Popowska, M. Entry Routes of Antibiotics and Antimicrobial Resistance in the Environment. In Antibiotics and Antimicrobial Resistance Genes: Environmental Occurrence and Treatment Technologies; Hashmi, M.Z., Ed.; Springer International Publishing: Cham, Germany, 2020; pp. 1–26. 35.
- da Costa, P.M.; Loureiro, L.; Matos, A.J. Transfer of multidrug-resistant bacteria between intermingled ecological niches: The interface between humans, animals and the environment. Int. J. Environ. Res. Public Health 2013, 10, 278–294. [CrossRef]
- Landers, T.F.; Cohen, B.; Wittum, T.E.; Larson, E.L. A review of antibiotic use in food animals: Perspective, policy, and potential. Public Health Rep. 2012, 127, 4–22. [CrossRef]
- Chancey, S.T.; Zähner, D.; Stephens, D.S. Acquired inducible antimicrobial resistance in Gram-positive bacteria. Future Microbiol. 2012, 7, 959–978. [CrossRef]
- Reygaert, W.C. An overview of the antimicrobial resistance mechanisms of bacteria. AIMS Microbiol. 2018, 4, 482–501. [CrossRef] [PubMed]
- Choi, U.; Lee, C.R. Distinct Roles of Outer Membrane Porins in Antibiotic Resistance and Membrane Integrity in Escherichia coli. Front. Microbiol. 2019, 10, 953. [CrossRef] [PubMed]
- Ghai, I.; Ghai, S. Understanding antibiotic resistance via outer membrane permeability. Infect. Drug Resist. 2018, 11, 523–530. [CrossRef] [PubMed]
- Dutt, Y.; Dhiman, R.; Singh, T.; Vibhuti, A.; Gupta, A.; Pandey, R.P.; Raj, V.S.; Chang, C.M.; Priyadarshini, A. The Association between Biofilm Formation and Antimicrobial Resistance with Possible Ingenious Bio-Remedial Approaches. Antibiotics 2022, 11, 930. [CrossRef]
- Van Acker, H.; Van Dijck, P.; Coenye, T. Molecular mechanisms of antimicrobial tolerance and resistance in bacterial and fungal biofilms. Trends Microbiol. 2014, 22, 326–333. [CrossRef]
- Ashley, R.E.; Dittmore, A.; McPherson, S.A.; Turnbough, C.L., Jr.; Neuman, K.C.; Osheroff, N. Activities of gyrase and topoisomerase IV on positively supercoiled DNA. Nucleic Acids Res. 2017, 45, 9611–9624. [CrossRef]
- Saha, M.; Sarkar, A. Review on Multiple Facets of Drug Resistance: A Rising Challenge in the 21st Century. J. Xenobiotics 2021, 11, 197–214. [CrossRef]
- Foster, T.J. Antibiotic resistance in Staphylococcus aureus. Current status and future prospects. FEMS Microbiol. Rev. 2017, 41, 430–449. [CrossRef]
- Wendlandt, S.; Shen, J.; Kadlec, K.; Wang, Y.; Li, B.; Zhang, W.J.; Feßler, A.T.; Wu, C.; Schwarz, S. Multidrug resistance genes in staphylococci from animals that confer resistance to critically and highly important antimicrobial agents in human medicine. Trends Microbiol. 2015, 23, 44–54. [CrossRef] [PubMed]
- Blair, J.M.; Webber, M.A.; Baylay, A.J.; Ogbolu, D.O.; Piddock, L.J. Molecular mechanisms of antibiotic resistance. Nat. Reviews. Microbiol. 2015, 13, 42–51. [CrossRef]
- Nikaido, H.; Pagès, J.M. Broad-specificity efflux pumps and their role in multidrug resistance of Gram-negative bacteria. FEMS Microbiol. Rev. 2012, 36, 340–363. [CrossRef]
- Poole, K. Efflux-mediated antimicrobial resistance. J. Antimicrob. Chemother. 2005, 56, 20–51. [CrossRef] [PubMed]
- Blair, J.M.; Richmond, G.E.; Piddock, L.J. Multidrug efflux pumps in Gram-negative bacteria and their role in antibiotic resistance. Future Microbiol. 2014, 9, 1165–1177. [CrossRef] [PubMed]
- Abushaheen, M.A.; Muzaheed; Fatani, A.J.; Alosaimi, M.; Mansy, W.; George, M.; Acharya, S.; Rathod, S.; Divakar, D.D.; Jhugroo, C.; et al. Antimicrobial resistance, mechanisms and its clinical significance. Dis. A-Mon. DM 2020, 66, 100971. [CrossRef]
- Chaw, P.S.; Höpner, J.; Mikolajczyk, R. The knowledge, attitude and practice of health practitioners towards antibiotic prescribing and resistance in developing countries-A systematic review. J. Clin. Pharm. Ther. 2018, 43, 606–613. [CrossRef]
- Chokshi, A.; Sifri, Z.; Cennimo, D.; Horng, H. Global Contributors to Antibiotic Resistance. J. Glob. Infect. Dis. 2019, 11, 36–42. [CrossRef]
- Klein, E.Y.; Van Boeckel, T.P.; Martinez, E.M.; Pant, S.; Gandra, S.; Levin, S.A.; Goossens, H.; Laxminarayan, R. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc. Natl. Acad. Sci. USA 2018, 115, E3463–E3470. [CrossRef]
- Van Boeckel, T.P.; Brower, C.; Gilbert, M.; Grenfell, B.T.; Levin, S.A.; Robinson, T.P.; Teillant, A.; Laxminarayan, R. Global trends in antimicrobial use in food animals. Proc. Natl. Acad. Sci. USA 2015, 112, 5649–5654. [CrossRef] [PubMed]
- Antibiotic Use in the United States, 2022 Update: Progress and Opportunities. Available online: https://www.cdc.gov/ antibiotic-use/stewardship-report/current.html (accessed on 10 November 2022).
- Michael, C.A.; Dominey-Howes, D.; Labbate, M. The antimicrobial resistance crisis: Causes, consequences, and management. Front. Public Health 2014, 2, 145. [CrossRef] [PubMed]
- Pulia, M.; Kern, M.; Schwei, R.J.; Shah, M.N.; Sampene, E.; Crnich, C.J. Comparing appropriateness of antibiotics for nursing home residents by setting of prescription initiation: A cross-sectional analysis. Antimicrob. Resist. Infect. Control 2018, 7, 74. [CrossRef]
- Woolhouse, M.; Waugh, C.; Perry, M.R.; Nair, H. Global disease burden due to antibiotic resistance-state of the evidence. J. Glob. Health 2016, 6, 010306. [CrossRef]
- Antibiotic Resistance: A Global Threat. Available online: https://www.cdc.gov/drugresistance/solutions-initiative/ stories/ar-global-threat.html (accessed on 10 November 2022).
- DiMasi, J.A.; Grabowski, H.G.; Hansen, R.W. Innovation in the pharmaceutical industry: New estimates of R&D costs. J. Health Econ. 2016, 47, 20–33. [CrossRef] [PubMed]
- Chang, Q.; Wang, W.; Regev-Yochay, G.; Lipsitch, M.; Hanage, W.P. Antibiotics in agriculture and the risk to human health: How worried should we be? Evol. Appl. 2015, 8, 240–247. [CrossRef]
- Animal production. Available online: https://www.fao.org/antimicrobial-resistance/key-sectors/animal-production/en/ (accessed on 12 November 2022).
- Castro-Sánchez, E.; Moore, L.S.; Husson, F.; Holmes, A.H. What are the factors driving antimicrobial resistance? Perspectives from a public event in London, England. BMC Infect. Dis. 2016, 16, 465. [CrossRef]
- Frost, I.; Van Boeckel, T.P.; Pires, J.; Craig, J.; Laxminarayan, R. Global geographic trends in antimicrobial resistance: The role of international travel. J. Travel Med. 2019, 26, taz036. [CrossRef]
- Arcilla, M.S.; van Hattem, J.M.; Haverkate, M.R.; Bootsma, M.C.J.; van Genderen, P.J.J.; Goorhuis, A.; Grobusch, M.P.; Lashof, A.M.O.; Molhoek, N.; Schultsz, C.; et al. Import and spread of extended-spectrum β-lactamase-producing Enterobacteriaceae by international travellers (COMBAT study): A prospective, multicentre cohort study. Lancet. Infect. Dis. 2017, 17, 78–85. [CrossRef]
- McCubbin, K.D.; Anholt, R.M.; de Jong, E.; Ida, J.A.; Nóbrega, D.B.; Kastelic, J.P.; Conly, J.M.; Götte, M.; McAllister, T.A.; Orsel, K.; et al. Knowledge Gaps in the Understanding of Antimicrobial Resistance in Canada. Front. Public Health 2021, 9, 726484. [CrossRef]
- Carter, R.R.; Sun, J.; Jump, R.L. A Survey and Analysis of the American Public’s Perceptions and Knowledge About Antibiotic Resistance. Open Forum Infect. Dis. 2016, 3, ofw112. [CrossRef] [PubMed]
- Antibiotic resistance. Available online: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance (accessed on 12 November 2022).
- Lin, T.Z.; Jayasvasti, I.; Tiraphat, S.; Pengpid, S.; Jayasvasti, M.; Borriharn, P. The Predictors Influencing the Rational Use of Antibiotics Among Public Sector: A Community-Based Survey in Thailand. Drug Healthc. Patient Saf. 2022, 14, 27–36. [CrossRef] [PubMed]
- Control, A. Global Governance to Tackle Antimicrobial Resistance: The Way Forward. Available online: http://resistancecontrol. info/2019-3/armed-conflicts-and-antimicrobial-resistance-a-deadly-convergence/ (accessed on 4 June 2023).
- Majumder, M.A.A.; Rahman, S.; Cohall, D.; Bharatha, A.; Singh, K.; Haque, M.; Gittens-St Hilaire, M. Antimicrobial Stewardship: Fighting Antimicrobial Resistance and Protecting Global Public Health. Infect. Drug Resist. 2020, 13, 4713–4738. [CrossRef] [PubMed]
- ]WHO. Global Action Plan on Antibiotic Resistance. Available online: https://www.emro.who.int/health-topics/drug-resistance/ global-action-plan.html (accessed on 12 November 2022).
- Assessing Non-Prescription and Inappropriate Use of Antibiotics Report on Survey. Available online: https://apps.who. int/iris/bitstream/handle/10665/312306/9789289054089-eng.pdf?sequence=1&isAllowed=y (accessed on 4 June 2023).
- Infection Prevention and Control. Available online: https://www.who.int/teams/integrated-health-services/infectionprevention-control (accessed on 12 November 2022).
- Implementation of Antibiotic Stewardship Core Elements at Small and Critical Access Hospitals. Available online: https://www.cdc.gov/antibiotic-use/core-elements/small-critical.html (accessed on 12 November 2022).
- Pinto Ferreira, J.; Battaglia, D.; Dorado García, A.; Tempelman, K.; Bullon, C.; Motriuc, N.; Caudell, M.; Cahill, S.; Song, J.; LeJeune, J. Achieving Antimicrobial Stewardship on the Global Scale: Challenges and Opportunities. Microorganisms 2022, 10, 1599. [CrossRef]
- Aidara-Kane, A.; Angulo, F.J.; Conly, J.M.; Minato, Y.; Silbergeld, E.K.; McEwen, S.A.; Collignon, P.J. World Health Organization (WHO) guidelines on use of medically important antimicrobials in food-producing animals. Antimicrob. Resist. Infect. Control 2018, 7, 7. [CrossRef]
- Mitchell, J.; Cooke, P.; Ahorlu, C.; Arjyal, A.; Baral, S.; Carter, L.; Dasgupta, R.; Fieroze, F.; Fonseca-Braga, M.; Huque, R.; et al. Community engagement: The key to tackling Antimicrobial Resistance (AMR) across a One Health context? Glob. Public Health 2022, 17, 2647–2664. [CrossRef]
- Othman, L.; Sleiman, A.; Abdel-Massih, R.M. Antimicrobial Activity of Polyphenols and Alkaloids in Middle Eastern Plants. Front. Microbiol. 2019, 10, 911. [CrossRef]
- Al-Amin, M.Y.; Lahiry, A.; Ferdous, R.; Hasan, M.K.; Kader, M.A.; Alam, A.K.; Saud, Z.A.; Sadik, M.G. Stephania japonica Ameliorates Scopolamine-Induced Memory Impairment in Mice through Inhibition of Acetylcholinesterase and Oxidative Stress. Adv. Pharmacol. Pharm. Sci. 2022, 2022, 8305271. [CrossRef]
- Foyzun, T.; Mahmud, A.A.; Ahammed, M.S.; Manik, M.I.N.; Hasan, M.K.; Islam, K.M.M.; Lopa, S.S.; Al-Amin, M.Y.; Biswas, K.; Afrin, M.R.; et al. Polyphenolics with Strong Antioxidant Activity from Acacia nilotica Ameliorate Some Biochemical Signs of Arsenic-Induced Neurotoxicity and Oxidative Stress in Mice. Molecules 2022, 27, 1037. [CrossRef]
- Islam, M.A.; Zaman, S.; Biswas, K.; Al-Amin, M.Y.; Hasan, M.K.; Alam, A.; Tanaka, T.; Sadik, G. Evaluation of cholinesterase inhibitory and antioxidant activity of Wedelia chinensis and isolation of apigenin as an active compound. BMC Complement. Med. Ther. 2021, 21, 204. [CrossRef]
- Mustafa, S.; Akbar, M.; Khan, M.A.; Sunita, K.; Parveen, S.; Pawar, J.S.; Massey, S.; Agarwal, N.R.; Husain, S.A. Plant metabolite diosmin as the therapeutic agent in human diseases. Curr. Res. Pharmacol. Drug Discov. 2022, 3, 100122. [CrossRef]
- Pawar, J.S.; Mustafa, S.; Ghosh, I. Chrysin and Capsaicin induces premature senescence and apoptosis via mitochondrial dysfunction and p53 elevation in Cervical cancer cells. Saudi J. Biol. Sci. 2022, 29, 3838–3847. [CrossRef]
- Kundo, N.K.; Manik, M.I.N.; Biswas, K.; Khatun, R.; Al-Amin, M.Y.; Alam, A.; Tanaka, T.; Sadik, G. Identification of Polyphenolics from Loranthus globosus as Potential Inhibitors of Cholinesterase and Oxidative Stress for Alzheimer’s Disease Treatment. BioMed. Res. Int. 2021, 2021, 9154406. [CrossRef]
- Amaning Danquah, C.; Minkah, P.A.B.; Osei Duah Junior, I.; Amankwah, K.B.; Somuah, S.O. Antimicrobial Compounds from Microorganisms. Antibiotics 2022, 11, 285. [CrossRef]
- Brives, C.; Pourraz, J. Phage therapy as a potential solution in the fight against AMR: Obstacles and possible futures. Palgrave Commun. 2020, 6, 100. [CrossRef]
- Dickey, S.W.; Cheung, G.Y.C.; Otto, M. Different drugs for bad bugs: Antivirulence strategies in the age of antibiotic resistance. Nat. Reviews. Drug Discov. 2017, 16, 457–471. [CrossRef] [PubMed]
- One Health Initiative. Available online: https://www.who.int/teams/one-health-initiative (accessed on 29 June 2023). 91. CDC. One Health Basics. Available online: https://www.cdc.gov/onehealth/basics/index.html (accessed on 29 June 2023).
- Van Camp, P.J.; Haslam, D.B.; Porollo, A. Prediction of Antimicrobial Resistance in Gram-Negative Bacteria from Whole-Genome Sequencing Data. Front. Microbiol. 2020, 11, 1013. [CrossRef]
- Anderson, M.; Clift, C.; Schulze, K.; Sagan, A.; Nahrgang, S.; Ait Ouakrim, D.; Mossialos, E. European Observatory Policy Briefs. In Averting the AMR Crisis: What Are the Avenues for Policy Action for Countries in Europe?: Copenhagen, Denmark, 2019.

